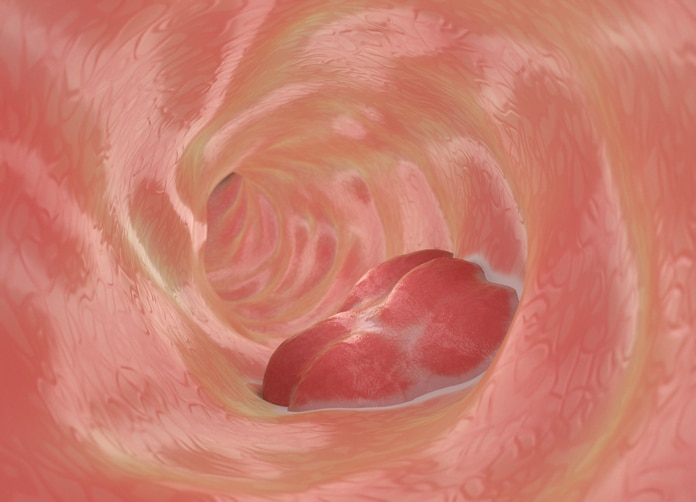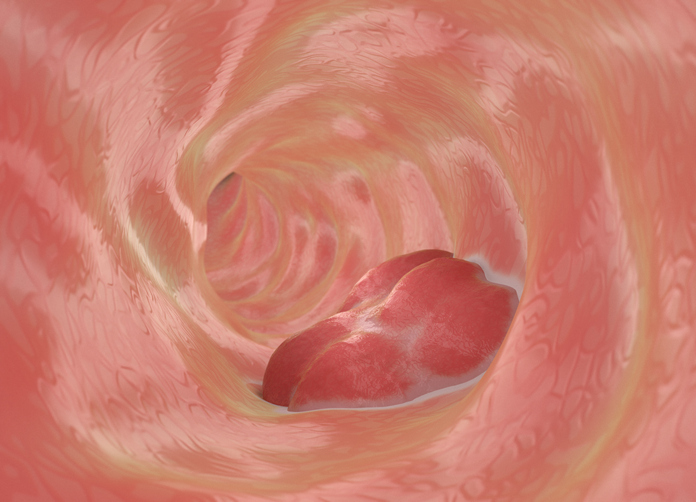
Colonoscopy screening intervals may be extended for people without a family history of colorectal cancer (CRC), studies suggest, allowing them to avoid unnecessary invasive tests.
The ten-year interval between examinations can be extended to 15 years if the first colonoscopy is negative for cancer, without significant negative results.
The study, published in JAMA OncologyAdds an evolutionary element that supports extending the historic 10-year screening interval for individuals at average CRC risk.
Mahdi Fallah, PhD, from the German Cancer Research Center in Heidelberg, and colleagues said: ‘This study provides evidence to recommend a longer colonoscopy screening interval than is currently recommended in most guidelines.
CRC is the third most common cancer and the second most common cause of cancer death worldwide.
Most colorectal cancer screening guidelines currently advocate a 10-year interval without colonoscopy, based on the time frame for a benign tumor to transform into carcinoma.
With emerging data suggesting this could be extended, the researchers studied the world’s largest comprehensive database of family cancer data.
Specifically, the team studied data from more than 110,000 people in Sweden who had no family history of CRC and had negative results at their first colonoscopy between the ages of 45 and 69.
A negative finding was defined as colorectal polyp, adenoma, carcinoma in situ, or undiagnosed colorectal cancer at first colonoscopy within 6 months before or after diagnosis.
These participants were compared with nearly two million matched control individuals who either did not undergo a colonoscopy during follow-up or underwent a colonoscopy that resulted in a CRC diagnosis.
During a maximum follow-up of 29 years, there were 484 CRC events and 112 CRC deaths in the group with negative colonoscopy findings, compared with 21,778 CRC cases and 552 CRC deaths in the control group.
Up to 15 years after the first colonoscopy with a negative result, the risk of CRC and CRC death remained lower than in control individuals.
The 10-year cumulative incidence of CRC at the 15th first negative colonoscopy was 72% among participants and control individuals. For CRC mortality, the 10-year cumulative risk was 55% of the control group.
Extending the screening interval from 10 to 15 years is estimated to result in only 2.4 additional CRC cases and 1.4 additional CRC deaths per 1000 individuals, eliminating one colonoscopy for each person in their lifetime.
Adding 15 to 16 years, or 20 years of screening, did not eliminate colonoscopies. In addition, it had the potential to increase harm, with missed CRC cases increasing from 2 to 4–12 per 1000 people, and CRC-specific mortality increasing from 1 to 2–4 deaths per 1000 people.
In a related opinion article, Rashid Lui and Andrew Chan, Ph.D., from the University of Hong Kong in China, question the 10-year “magic number.”
“Taken together, these data suggest that 15 years after colonoscopy with negative results may be the optimal time for screening,” they write.
However, Lui and Chan note that the study was based on data collected in the European population.
“Confirmation of these results in other settings is critical to generalizing these findings globally, including parts of the world such as Asia, where large-scale CRC screening has recently begun,” they added.
“Not only is the adenoma-carcinoma sequence time different in non-European populations, but differences in CRC background incidence significantly affect the number of CRCs prevented at a given screening time.”