By Cassidy Morrison Senior Health Reporter for Dailymail.Com
13:55 10 February 2024, Updated 14:24 10 February 2024
- As the temperature of the climate increases, the fungi that cause infections are becoming more widespread
- People with a fungal infection in the lungs seem to have pneumonia at first
- Read more: 29-year-old Michigan man dies after contracting deadly fungal infection
The death of a Michigan chef from a fungal infection has shed light on a silent epidemic that has been growing in America for years.
Four deadly species in particular have become more common over the past few decades. Infecting thousands of people Now compared to just a dozen in the early 2000s.
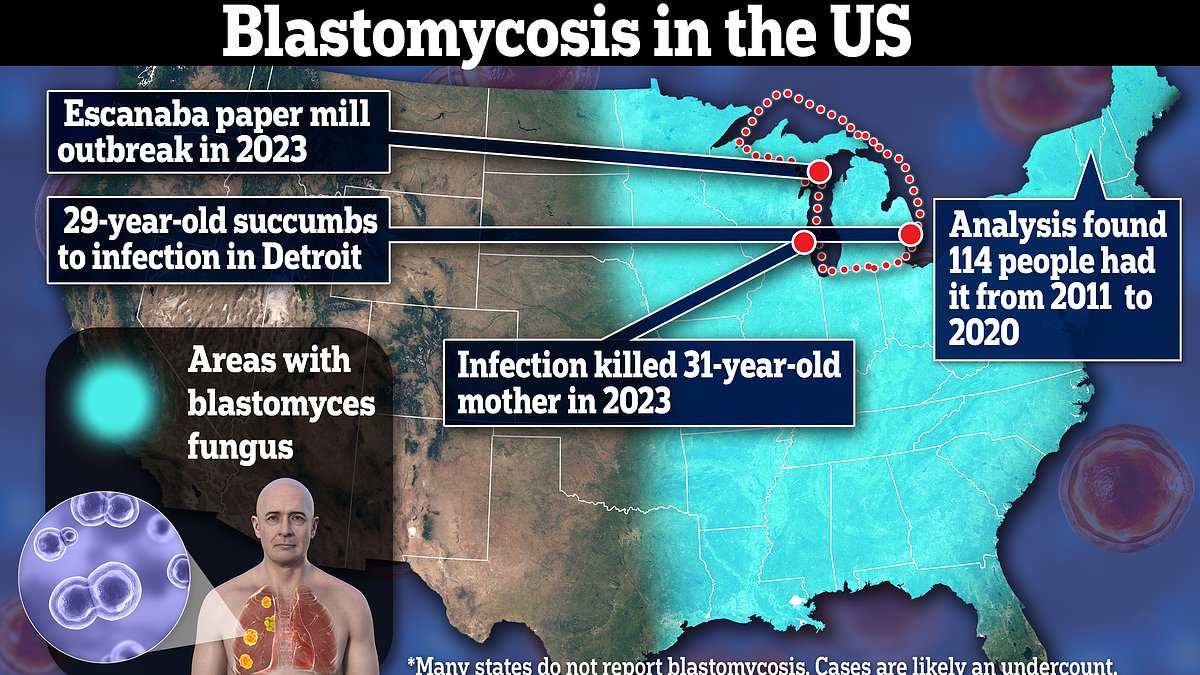
DailyMail.com revealed earlier this week that 29-year-old Ian Pritchard, the latest victim of the outbreak, had his lungs ‘ravaged’ by Blatomycosis – a microscopic yeast that is spread when people inhale its spores.
The fungus hides in moist soil and rotting wood in the upper Midwest, but the warming climate has allowed it to flourish on the East Coast as well.
Meanwhile in the West, valley fever is sickening more people than ever before, with California cases tripling from 2014 to 2018 and from 2018 to 2022.
After reporting on Ian Pritchard’s death, DailyMail.com has heard from several other people who have either loved them or themselves fallen victim to deadly fungal infections.
The Centers for Disease Control and Prevention and the World Health Organization have raised warnings in recent years about fungal pathogens that can evade drugs.
Climate change combined with international travel makes the introduction of potentially dangerous pathogens, including fungal species, more likely.
Supposedly 7,199 died of fungal diseases. It happened in 2021, according to the CDC. This is up from 5,922 deaths and 4,833 deaths a year ago.
Ian Pritchard’s case of Blatomycosis was one of the first reported in the US in 2024. His cousin Lorelei Walker detailed the extent of her injuries to DailyMail.com. Ian is the second member of her family to be ravaged by the disease.
She told DailyMail.com: ‘Ian is the second in my family to have succumbed to the disease. If I hadn’t gone through it with my husband, I would never have known what this disease is and what it does – not only to the person fighting it, but to the family and friends who watch it.’
Fungi that hide in moist soil, leaves, and rotting wood release explosives into the air when disturbed, which can penetrate tissue and cause infection. For example, the fungus that causes blatomycosis transforms itself into a type of yeast that reproduces in the lungs and causes infection.
Mrs Walker still does not know how her husband – who has underlying kidney disease – contracted it in June 2020. Ira was rushed to the hospital from his dialysis session in June 2020 at the height of the global covid pandemic. After weeks of shortness of breath, fatigue and muscle aches.
An X-ray showed a benign mass that suggested to doctors that he had pneumonia, even though his condition did not respond to standard treatment for a lung infection.
He was admitted to the hospital, and subsequent tests confirmed blatomycosis.
Diagnosing Blastomycosis requires a chest X-ray or CT scan to identify lung masses or cavities. Doctors also take fluid or tissue samples to check for yeast cells that change when blastomycosis enters the lungs.
Ira spent a month in a hospital after doctors surgically repaired a hole in his neck leading to a tube before he was transferred to a specialist facility for advanced treatment. Despite his hopes of regaining his lost strength and muscle mass, his condition worsened.
As she told DailyMail.com: ‘Instead of gaining strength, he became weaker. Every time the hospital called, there was news of another setback.
At the end of September, he got a call from his sister telling me he had decided to come home under hospice care.
She put the phone to his ear to confirm. A few days later I spoke to the case manager and arranged for him to come home.’
Studies have shown that warmer climates create a more hospitable environment for many of the worst types of fungi and can even help them mutate in ways that cannot be treated with standard medications.
The fungus that causes valley fever, Coccidioides, thrives in hot desert areas, which are constantly hot and dry. And another, Histoplasma, which causes histoplasmosis, grows in the wet soil on the east coast, which is getting more rain as the years go by.
In an ever-changing environment that allows fungi to thrive and adapt, there is a risk that current antifungal treatment tools will fail as health care workers battle a growing crisis of untreatable pathogens.
Neither Ms. Walker nor Pritchard’s loved ones could say where they were exposed, but Blastomyces thrives in moist soil and humid environments, so it was likely outdoors.
The Midwest has warmed, and storms are getting stronger. Rainfall has increased by 20 percent in some areas since 1900.
Average winter temperatures in the U.S. have risen by about three degrees, and spring temperatures by about two degrees. In balmier climates, fungi have a longer growing season, allowing them to reproduce longer and more widely.
Fungi are able to migrate to new areas that were unsuitable decades ago. Vermont, a state where Blatomyces is not seen as endemic, has become the new home of the fungus.
Earlier this year, Vermont health officials and the Centers for Disease Control and Prevention combed insurance claims to find cases of Blatomycosis that the state is not required to report.
exposed 114 residents infected with the virus. Of these 114 diagnoses, 30 had one or more hospitalizations associated with baltomycosis, and four died from the virus.
Massachusetts does not have to report cases of blastomycosis to the federal government either. It was there that 60-year-old Darcy Coderre became seriously ill with what her doctors first diagnosed as pneumonia.
In the year When she first presented to doctors in 2016, they believed the mark on her lung was cancer. It was only after a biopsy that doctors realized they were actually dealing with a case of blastomycosis.
She said: ‘My doctor was shocked. He said he hasn’t seen a case of that in Massachusetts.
‘We tried to find out where he got it from and couldn’t figure it out. I thought that the garden, so we can be from the soil. I walk, but I stay on the trails.’
Antifungal medicine worked, and she recovered, but she still has two scars from the infection. She also now has asthma, which she believes is a permanent result of her illness.
Another dangerous fungus is on the rise, but its connection to climate change is more murky. Instead, Candida auris strains are associated with hospital settings where they can spread rapidly, particularly among residents of long-term care facilities or among people with indwelling devices — such as catheters, tracheostomies, or wound drains — or on mechanical ventilators.
Candida auris is an acute global health concern, and is increasing annually in the US.
Federal government surveillance shows about 60 infections in the U.S. from 2013 to 2016, but there were more. 2,300 cases in 2022 alone.
Antifungal medication may not be effective. Some C auris infections are resistant to all three antifungal drugs: azoles, echinocandins, and amphotericin B. Echinocandins are the first line of therapy to treat C auris.
In recent years, multidrug-resistant strains of Cauris have become more common.